30 Nov Steps in the sterilisation process
Sterilisation is a process consisting of individual phases (from decontamination to use of RMDs and surgical instruments): each step is relevant, not performing it or performing it incorrectly compromises the entire process and exposes the patient, the operator and the facility to potential hazards.
It is important to use adequate and effective technologies, in line with the reference standards.
Collection and transport of the material to be processed: RMDs and surgical instruments
After its use, the contaminated material is immediately immersed in a decontaminating liquid and transported to a zone/area dedicated to the next steps: generally the CSSD.
Decontamination and Washing of RMDs
Decontamination and washing can be automatic or manual.
Automatic mode, suitably certified and guaranteed, is generally preferred. Washing of RMDs is an essential prerequisite for effective action in the subsequent stages and must take place in a dedicated, equipped area/space away from the packaging area of RDMs.
After the washing procedures, a thorough rinse with running water, possibly demineralised, is also carried out in order to remove all traces of detergent from the RMD.
Washing with appropriate instruments is referred to as medical device disinfection.
Disinfection of a medical device takes place after washing and allows to significantly reduce the presence of bacteria, preparing the device for the next stage, sterilisation, under the best possible hygienic conditions.
Drying, control, testing and maintenance of the RMD
Drying is essential: the presence of moisture on the surface of RMDs compromises the sterilisation process as it encourages the natural growth of microorganisms.
After the washing and drying processes and before packaging, it is important to check the integrity and functionality of the surgical instrument being sterilised.
Packaging of the RMD prior to the sterilisation process
Packaging is the activity of placing RMDs in a sterile barrier system (SBS) prior to sterilisation: this allows sterility to be maintained, after the autoclave process, until their reuse.
There are different types of SBSs (single-use and multi-use) and they are appropriately selected according to the sterilisation method and the type and weight of the RMDs they are to house in the sterilisation process.
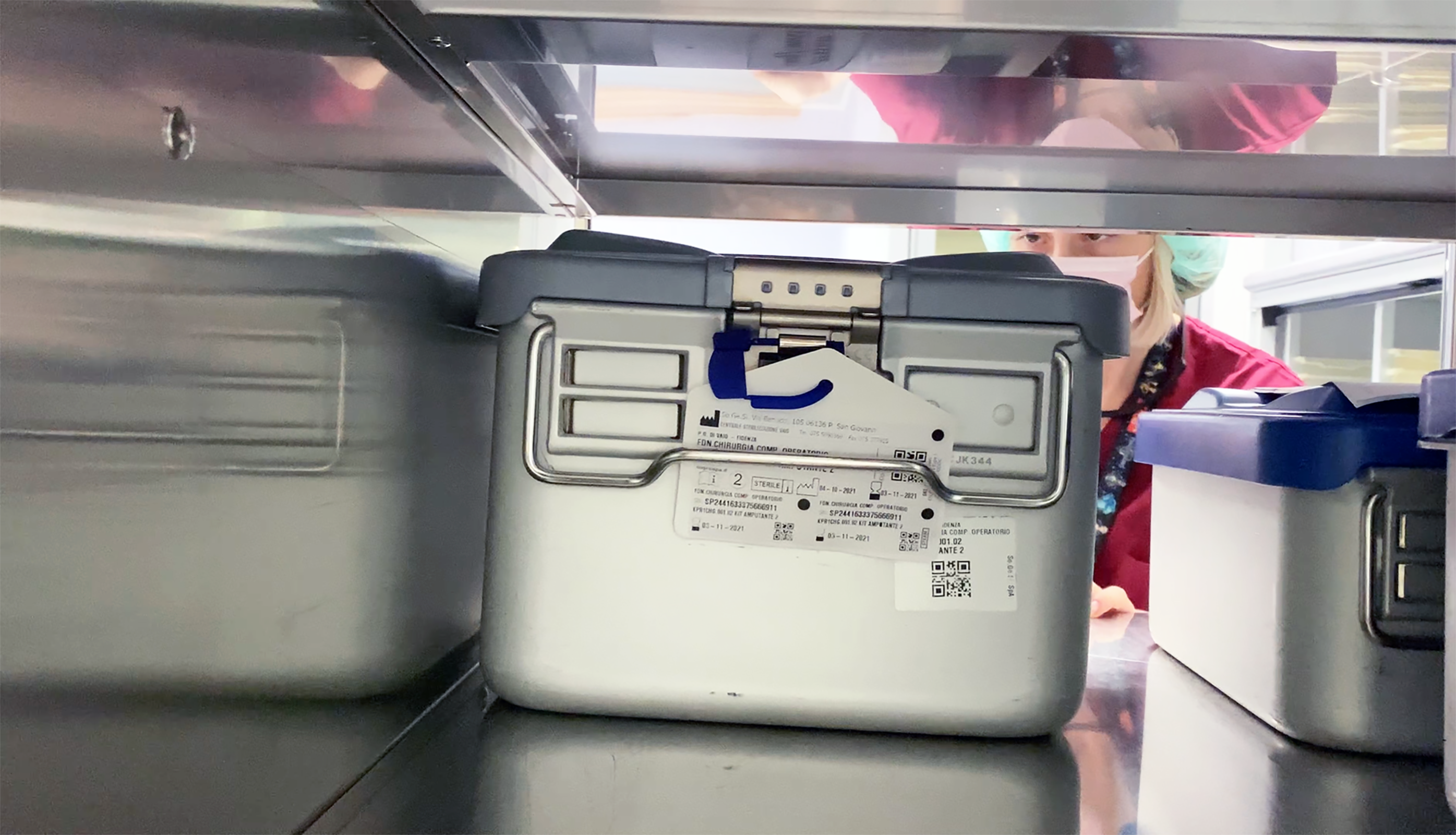
Labelling and Traceability
All SBS packages must be labelled. The label must contain all the data necessary to register the sterilisation batch that will undergo the process: only when this is validated will the batch be guaranteed sterile.
Thanks to a traceability system, the data contained on the label and which uniquely identifies the sterilisation batch is recorded.
It is therefore possible to follow the process of a specific MD, check all the critical elements that characterise the process it has undergone, and identify the patient on whom the MD has been used.
The sterilisation phase: which sterilization method to use?
There are different sterilisation methods, depending on the sterilising agent used. Knowing the most appropriate treatment techniques, taking into account the nature of the instrument and its intended use, is the first variable in choosing the most suitable type of sterilisation.
The most commonly used sterilisation methods are:
• Sterilisation with saturated steam
• Sterilisation with hydrogen peroxide ( hydrogen autoclave) or plasma gas
• Sterilisation with peracetic acid
• Sterilisation with ethylene oxide
• Sterilisation with formalin
Depending on the material or type of surgical instrument and RMD to be subjected to the sterilisation process, one method may be more appropriate than another.
Each of these sterilisation methods reflects characteristics that determine their effectiveness in the infection prevention and control process.
Some of the chemical methods have contraindications due to the sterilising agents used (toxic or highly dangerous to health) and over the years have been increasingly replaced (or severely restricted by law) by sterilisation methods that are safer for both operators and patients.
High-temperature saturated steam sterilisation is the technique that exploits the sterilisation potential of high-temperature steam.
Flowing steam (Koch steamer) or saturated steam (autoclave) eliminates microorganisms by denaturing their proteins and other biomolecules.
Sterilisation by autoclave is the most widely used method, as it is very effective due to its good steam penetration capacity, as well as being inexpensive and non-toxic, and applicable to a large number of materials and instruments.








No Comments